Lilian Nguyen, Rebecca Kim, Lillian Thai, Ysabella Ballesteros-Barajas, Andrea Romero

Our study investigates language barriers’ impact on patient-physician relationships among marginalized racial and ethnic communities in Southern California. We aim to understand how limited English proficiency affects healthcare access and quality for non-native English speakers. This exploration is crucial in identifying and addressing disparities in healthcare settings, particularly how language barriers intensify existing challenges. We hypothesize that disparities in language proficiency significantly influence the quality of care received by ethnically marginalized patients. Our research highlights ongoing societal norms in America, which disproportionately affect immigrants. We emphasize the necessity of addressing healthcare disparities for ethnically marginalized communities, advocating for enhanced resources and support. Analysis of data patterns reveals the profound impact of limited English proficiency on patient understanding and comfort in medical settings. Additionally, we identify the added responsibilities shouldered by non-English patients and the minimization of patient-physician interaction in the US healthcare system. In conclusion, our findings underscore the urgency of improving communication and understanding between patients and providers. This entails training healthcare providers in cultural competency and ensuring multilingual health materials’ availability. By addressing language barriers, we can strive towards a more equitable healthcare system that meets the diverse needs of all patients.
Introduction and Background
Our study explores the intricacies of patient-doctor relationships, with a specific focus on the ramifications of language barriers among individuals from marginalized racial and ethnic communities in California. Our objective is to comprehend how language proficiency, particularly among non-native English speakers, impacts their interactions with healthcare providers and their ability to access healthcare resources. This research holds significance in unveiling the challenges faced by these communities in healthcare settings, particularly how language barriers may exacerbate these challenges. Furthermore, we aim to explore the influence of language on the quality of care. Our hypothesis suggests that disparities in language proficiency between physicians and patients from ethnically marginalized communities significantly influence the quality of healthcare received. We seek to address the question: “Does language proficiency between physicians and patients from ethnically marginalized communities impact the quality of care?”
The ongoing Eurocentric-centric societal norms in America, profoundly affecting immigrants and refugees who have migrated to the country since the 20th century (Batlova 2018), have sparked discussions on the interpersonal and intrapersonal repercussions within marginalized communities. During this period, many immigrant groups encountered social and economic marginalization in American society, leading to their disconnection from the healthcare system (Anderson 2019). Our research endeavors to explore these effects within the framework of the US healthcare landscape, dissecting how the experiences of minority groups may differ from those of predominant communities through the analysis of language usage and conversations. Healthcare holds paramount importance for the living conditions of these burgeoning populations, as unequal access to adequate resources may jeopardize their overall well-being (Hsueh 2021). Previous studies have indicated physician bias as a limiting factor in physician-patient understanding, thus fueling ethnic disparities within healthcare settings.
Additionally, minority populations, including Hispanic, Black, and Asian communities, are expected to account for 40% of the US population by 2035 and 47% by 2050 (Cooper 2003). Therefore, as minority populations in America continue to grow (Cooper 2003), it becomes increasingly imperative to strive towards enhancing their quality of care by addressing potential barriers to access.
Hence, this research aims to further emphasize the correlations between English language proficiency and the quality of care in physician-patient relationships in America. Paying attention to recurrent themes in word choices used by participants will aid in highlighting how one’s ethnic identity may contribute to communication barriers (Irvine 2020). The selection of words by our participants when responding to questions regarding their relationship with their primary healthcare provider remains crucial in understanding their healthcare experiences and evaluating the quality of care they receive. This is because self-reported health status is imperative in raising awareness of vulnerable minority communities and their access to quality healthcare (Gandhi 2020). Analyzing recurrent themes in word choices will, therefore, offer a more nuanced insight into how ethnic identity influences communication barriers.
Methods
Our study investigates the impact of language barriers on patient-doctor relationships within marginalized communities, focusing on healthcare quality, resource access, and patient vulnerability. Employing a mixed-methods approach, we utilize surveys and structured interviews to gather data from individuals across diverse marginalized racial and ethnic backgrounds with varying English proficiency levels. The survey involves five participants from the target population, while in-depth interviews are conducted with another group of five individuals. Both methodologies are guided by specific formulated questions. Data collection occurs via online platforms for surveys and virtual or in-person settings for interviews, ensuring demographic diversity. Sampling aims to encompass individuals from various marginalized racial and ethnic backgrounds with differing English proficiency levels. Quantitative survey data is analyzed using Google Forms, while qualitative interview data is scrutinized for analysis.
Results
Discussion and Conclusions
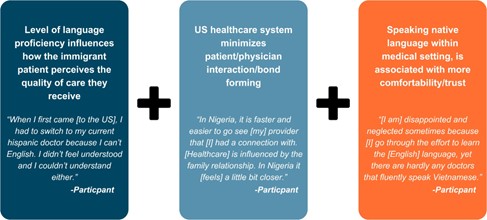
Upon analyzing our data, we have uncovered several underlying patterns (Figure 3).
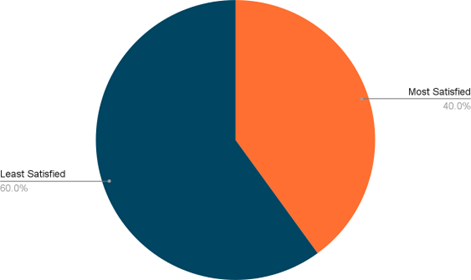
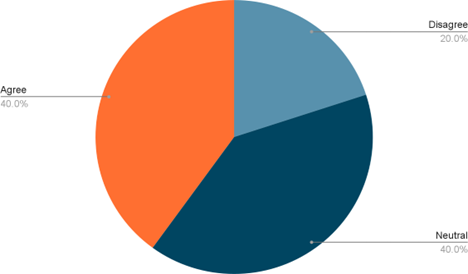
Participants were tasked with evaluating their comprehension of the information and instructions provided by their medical providers. A notable observation was made by several participants who, while generally able to understand this information, encountered challenges in comprehending medical terminology that they are only familiar with in their native language (Figure 1). Consequently, our findings indicate a strong positive correlation between limited English proficiency and difficulties in understanding medical information. This correlation is particularly significant for immigrant patients who already face additional social and cultural barriers, such as cultural assimilation. Speaking in their native language with their primary care physician fosters a sense of familiarity and comfort (Figure 2). Additionally, ethnically marginalized patients who communicate in their native language with their physician feel more at ease expressing themselves and discussing sensitive health issues without fear of misunderstanding or judgment.
Moreover, we explored the ways in which patients may assume extra responsibility or seek support regarding their medical care. While some participants reported not assuming any additional responsibility, others mentioned making efforts to learn English to communicate with their English-speaking doctors or relying on family members for support during medical visits. This highlights the burden placed on non-English patients to bridge communication gaps with their physicians.
Furthermore, our study reveals a significant finding regarding the minimization of patient-physician interaction in the US healthcare system (Figure 3). Despite acknowledging advancements and modernity in US medicine compared to their countries, our data indicates a minimization of interaction and bonding. This may be attributed to factors such as limited appointment times, a national physician shortage, minimal physician cultural sensitivity, and an overarching focus on efficiency over personalized care (Silver 2019). Consequently, ethnically marginalized patients may feel disconnected from their healthcare providers, perceiving a lack of empathy and understanding during medical encounters.
In conclusion, our study underscores the necessity for additional resources and support for marginalized communities with limited English proficiency to achieve the same level of quality communication and care as native English speakers. Moreover, our research highlights significant health disparities among ethnically marginalized communities with limited English proficiency. This emphasizes the importance of addressing these disparities and implementing improvements in the healthcare system. Immigrants, in particular, face the challenge of mastering language, culture, and healthcare protocols to engage with providers and comprehend health information (Radl-Karimi 2020). Healthcare providers must receive training in cultural competency, health literacy, and patient education techniques. Additionally, ensuring the availability of health materials in multiple languages and formats tailored for low-literacy populations is crucial. Our study also reveals that participants sought assistance in understanding medical instructions when provided with written reference materials after their visits. By enhancing communication and understanding between patients and providers, we can strive towards a more equitable healthcare system that caters to the diverse needs of all patients.
References
Anderson, K. M., & Olson, S. (2019). Immigration as a Social Determinant of Health Proceedings of a Workshop. National Academies Press.
Batalova, J., & Alperin, E. (2018, September 13). Vietnamese immigrants in the United States. Migration Policy Institute. https://www.migrationpolicy.org/article/vietnamese-immigrants-united-states-5
Cooper, L. A., & Roter, D. L. (1970, January 1). Patient-provider Communication: The Effect of Race and Ethnicity on Process and Outcomes of Healthcare. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. https://www.ncbi.nlm.nih.gov/books/NBK220354/
Gandhi, K., Lim, E., Davis, J., & Chen, J. J. (2020, January). Racial-ethnic disparities in self-reported health status among US adults adjusted for sociodemographics and multimorbidities, National Health and Nutrition Examination Survey 2011-2014. Ethnicity & health, 25(1), 65-78. https://pubmed.ncbi.nlm.nih.gov/29092622/
Hsueh, L., Hirsh, A. T., & Stewart, J. C. (2019, July 10). Patient–provider Language Concordance and Health Outcomes: A Systematic Review, Evidence Map, and Research Agenda. Medical Care Research and Review, 78(1), 3-23. https://journals.sagepub.com/doi/10.1177/1077558719860708
Irvine, F. E., Roberts G. W., Jones, P., Spencer L. H., Baker C. R., & Williams C. (2006, January 31). Communicative Sensitivity in the Bilingual Healthcare Setting: A Qualitative Study of Language Awareness. Journal of Advanced Nursing, 53(4), 422-434. https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2648.2006.03733.x
Radl-Karimi, C., Nicolaisen, A., Sodemann, M., Batalden, P., & von Plessen, C. (2020). Under what circumstances can immigrant patients and healthcare professionals co-produce health? – An Interpretive Scoping Review. International journal of qualitative studies on health and well-being, 15(1), 1838052. https://doi.org/10.1080/17482631.2020.1838052.
Silver, J. K., Bean, A. C., Slocum, C., Poorman, J. A., Tenforde, A., Blauwet, C. A., Kirch, R. A., Parekh, R., Amonoo, H. L., Zafonte, R., & Osterbur, D. (2019). Physician Workforce Disparities and Patient Care: A Narrative Review. Health equity, 3(1), 360–377. https://doi.org/10.1089/heq.2019.0040.